HTML
Opinion - (2022) Volume 12, Issue 6
Significant Cost Effectiveness of Antibiotics
Jan Krestos**Correspondence: Jan Krestos, Department of Biotechnology, Mekelle University, Mekele, Ethiopia, Email:
Received: 10-Nov-2022, Manuscript No. IJP-22-85040; Editor assigned: 14-Nov-2022, Pre QC No. IJP-22-85040 (PQ); Reviewed: 25-Nov-2022, QC No. IJP-22-85040; Revised: 08-Dec-2022, Manuscript No. IJP-22-85040 (R); Published: 16-Dec-2022, DOI: 10.37532/2249-1848.2022.12(6).25
Description
Policymakers and healthcare payers are concerned about the cost effectiveness of antibiotics due to rising healthcare expenses and a lack of resources. The purpose of this study is to identify and show the elements influencing the cost effectiveness of antibiotic treatment for bacterial illnesses by drawing on existing economic analyses. The results show that both external and internal factors (such as diagnosis, comparative costs and comparative effectiveness, resistance, patient compliance with treatment, and treatment failure) have an impact on the cost effectiveness of antibiotics (i.e., funding source, clinical pharmacy interventions, and guideline implementation interventions). When recommending an antibiotic, doctors must consider these characteristics and determine whether a particular antibiotic treatment adds enough value.
Patients who experience bacterial illnesses now enjoy better health thanks in large part to antibiotics. For instance, lower respiratory tract infections are frequently treated with antibiotics. In patients with acute exacerbations of community-acquired pneumonia and COPD, antibiotic therapy is advised by scientific literature and international guidelines (CAP). Additionally, in patients with a microbiological diagnosis of bacterial infection or severe sickness, antibiotics seem useful in increasing cure rates and reducing the duration of acute sinusitis. Antibiotics' extra benefits for therapeutic and preventative purposes are so compelling, in fact, that many older antibiotics were never subjected to controlled clinical studies. Policymakers and healthcare payers are worried about the cost effectiveness of antibiotics in a time of rising healthcare expenses and constrained resources. Economic evaluation is a technique that examines if antibiotic therapy contributes to health in a way that justifies its expenses in order to determine whether antibiotics are cost-effective. A comparative review of at least two health technologies' costs and results is what is referred to as a "economic evaluation."
A number of stakeholders can utilise information on the cost effectiveness of antibiotic therapy of bacterial illnesses to make decisions. Economic analysis can help policymakers allocate the limited resources for healthcare. Evidence about cost effectiveness is being used by health care payers in an increasing number of nations to guide decisions about drug pricing and reimbursement. Better cost-effective antibiotics are rewarded with a more favourable pricing or reimbursement. Economic analysis can be used by healthcare providers to learn more about different ways to treat bacterial infections. Finally, pharmaceutical corporations can use economic evaluation methodologies to show that their antibiotics are cost-effective.
The literature has several economic analyses that evaluate the cost-effectiveness of treating bacterial illnesses with antibiotics. This study aims to pinpoint and analyse the variables influencing antibiotics' cost-effectiveness. The National Health Service Economic Evaluation Database, Health Technology Assessments Database, Cochrane Database of Systematic Reviews, and EconLit databases of the Centre for Reviews and Dissemination, were searched to find economic assessments. The bibliographies of the listed papers were further searched for additional pertinent studies. The phrases "pharmaco-economics," "economic evaluation," "cost effectiveness," "cost minimization," "cost utility," and "cost benefit" alone and in combination with one another were related to various illness kinds and antibiotic classes. The National Health Service Economic. The bibliographies of the listed papers were further searched for additional pertinent studies. The phrases "pharmaco-economics," "economic evaluation," "cost effectiveness," "cost minimization," "cost utility," and "cost benefit" alone and in combination with one another were related to various illness kinds and antibiotic classes.
Because antibiotic treatment methods and the structure and funding of healthcare systems are anticipated to change over time, earlier research were thought to be of limited practical significance. Included were both original economic analyses and literature studies of economic analyses. Factors relating to the properties and use of antibiotics (i.e., diagnosis, comparative costs and comparative effectiveness, resistance, patient compliance with treatment, and treatment failure) as well as external factors have an impact on the cost effectiveness of antibiotic treatment of bacterial infections (i.e., funding source, clinical pharmacy interventions, and guideline implementation interventions)
Since a patient's self-reported clinical symptoms are typically used to make the diagnosis of a bacterial infection, this makes it challenging. The example of COPD flare-ups serves as a good illustration of this. Because COPD exacerbations can be varied and there is disagreement about what constitutes an exacerbation, diagnosing one can be challenging. Furthermore, it is not always possible to obtain high-quality sputum specimens in practise. This suggests that proper treatment is not always provided and that exacerbations are not always recognised as such. In fact, there is proof that when utilising a symptom-based definition, a healthcare professional misses up to 50% of exacerbations.
A Spanish economic analysis revealed that, in terms of determining the bacterial aetiology, the most effective treatment method for CAP depended on the bacterial pathogen involved, and the doctor required to tailor the antibiotic treatment strategy to the cause. If the doctor was able to distinguish clinically the bacterial aetiology, the authors found that amoxicillin 1 g for treating CAP was more efficient and less expensive than moxifloxacin, telithromycin, or clarithromycin. Moxifloxacin became the best choice if the doctor needed to start empirical treatment without knowing the isolate's antibiotic susceptibility profile or the pathogen that was causing it. However, because the model of treatment routes in this study had to be rudimentary, further modelling in this area is not recommended.
Manuscript Submission
Submit your manuscript at Online Submission System
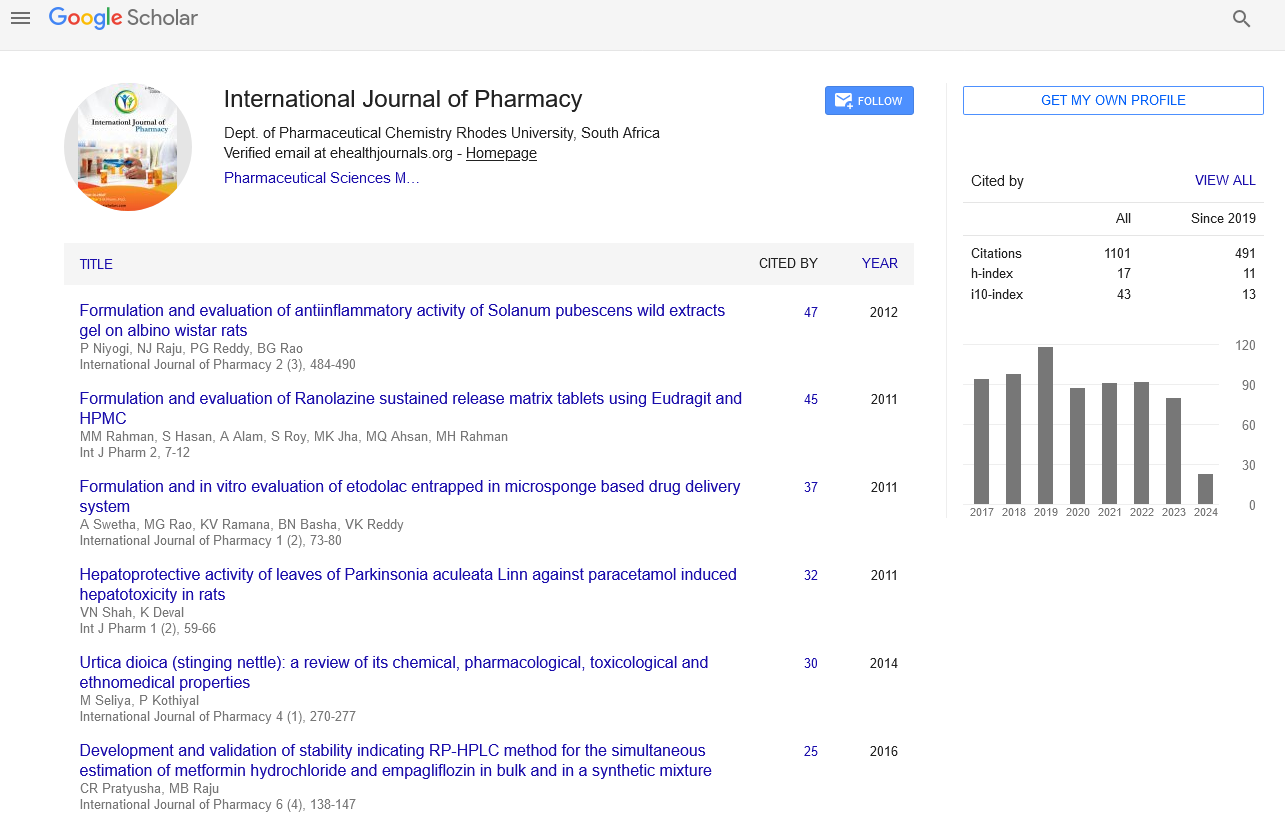
Google scholar citation report
Citations : 1101
International Journal of Pharmacy received 1101 citations as per google scholar report
International Journal of Pharmacy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- HINARI
- Index Copernicus
- Google Scholar
- The Global Impact Factor (GIF)
- Polish Scholarly Bibliography (PBN)
- Cosmos IF
- Open Academic Journals Index (OAJI)
- Directory of Research Journal Indexing (DRJI)
- EBSCO A-Z
- OCLC- WorldCat
- MIAR
- International committee of medical journals editors (ICMJE)
- Scientific Indexing Services (SIS)
- Scientific Journal Impact Factor (SJIF)
- Euro Pub
- Eurasian Scientific Journal Index
- Root indexing
- International Institute of Organized Research
- InfoBase Index
- International Innovative Journal Impact Factor
- J-Gate