HTML
Opinion Article - (2022) Volume 12, Issue 2
Short Note on Occurrence of Hysteria Paralysis after Cervical Nerve Root Block Treatment
Dilshuk Begum**Correspondence: Dilshuk Begum, Department of Pharmacy, University in Bologna, Bologna, Italy, Email:
Received: 07-Feb-2022, Manuscript No. IJP-22-60662; Editor assigned: 11-Feb-2022, Pre QC No. IJP-22- 60662(PQ); Reviewed: 21-Feb-2022, QC No. IJP-22-60662; Revised: 28-Feb-2022, Manuscript No. IJP-22- 60662(R); Published: 07-Mar-2022, DOI: 10.37532/2249-1848-22.12.07
Description
Hysterical paralysis should be diagnosed with caution, especially following treatment. Conversion disorders have been recognised in medical practise for millennia, but little is understood about the underlying cognitive and emotional processes, as well as the neurophysiological foundations. The existence of neurological symptoms (such as paralysis, anaesthesia, blindness, and so on) that cannot be attributed to organic brain injury but appear to be triggered by specific emotional stressors or conflicts is termed as conversion.
It is frequently linked to a traumatic or social incident, with discomfort in the affected "Paralyzed" part. After examining the protagonist in this case, we discovered that she was economically poor, had a limited education, and had difficulties expressing her grief. In his 50 years, her father died of hemiplegia. Before therapy, she had discomfort in her right arm and lower extremity, and after treatment, she had numbness and nerve conduction abnormalities produced by local anaesthetic medicines, which broke up her emotions and caused worry.
Even yet, the formation of hysteria paralysis is a possibility. The back of her disability is the same as her father's hemiplegia from a brain infarction. Many times, computed tomography, magnetic resonance imaging, and electrodiagnostic investigations are employed to define normal. Pain medication is mainly used to treat peripheral nerve blocks. Low concentrations of topical anaesthetics can successfully stop the pain cycle.
In the innervated area, compound vitamin B12 and a little dose of steroid can reduce neuroinflammation and alleviate muscular tissue fatigue. Visual ultrasound can distinguish peripheral injection, intraneural injection, or nerve bundle injection, however even intraneural injection does not always result in nerve injury, and the appearance of such visualisation cannot lessen the risk of nerve injury.
Is this to say that nerve harm is not caused by intraneural injection? One of the causes of peripheral nerve damage has been identified as ischemia. Acute decreases in peripheral nerve blood flow were observed after topical application of local anaesthetic to the rat sciatic nerve, but no substantial histological alterations were observed. Exposure to excessive concentrations or doses of local anaesthetics causes direct neurotoxicity. Despite the fact that all local anaesthetics have some neurotoxic potential, ropivacaine is expected to be less hazardous than other drugs like lidocaine.
Furthermore, because of the steroid, introvescular injection can induce major complications. Blood in the needle hub was found to be 97 percent specific but only 45.9% sensitive in predicting intravascular injections. It was discovered that repeated aspiration during drug injection can boost the rate of steroid detection in the blood. Steroid infusions frequently result in major consequences, particularly when particles lodge in blood arteries, resulting in catastrophic complications such as spinal cord and brain infarction. Graham looked at the cervical intervertebral foramen of 1340 patients and discovered 78 incidences of ridge plug in various sections of the body, including the brain and spinal cord.
In 24 hours, magnetic resonance imaging can locate the violation. When dealing with a paralysed patient, imaging and electrophysiological testing are frequently required, but they are pricey. The results of our MRI were normal. Electromyography of muscles and nerves was consistent with those before the procedure, ruling out nerve block and steroid intravascular injection problems. The point of hysterical paralysis was well stated. According to studies, hysterical paralysis takes about 6 months to fully recover, and some individuals still have pain.
In this situation, we used anti-anxiety and anti-depressant medications as well as rehabilitation therapy. In three weeks, the patient's muscle strength had fully restored. Traditional Chinese medicine also uses Yongquan acupoint stimulation therapy. In this case, we used a combination of these methods.
Manuscript Submission
Submit your manuscript at Online Submission System
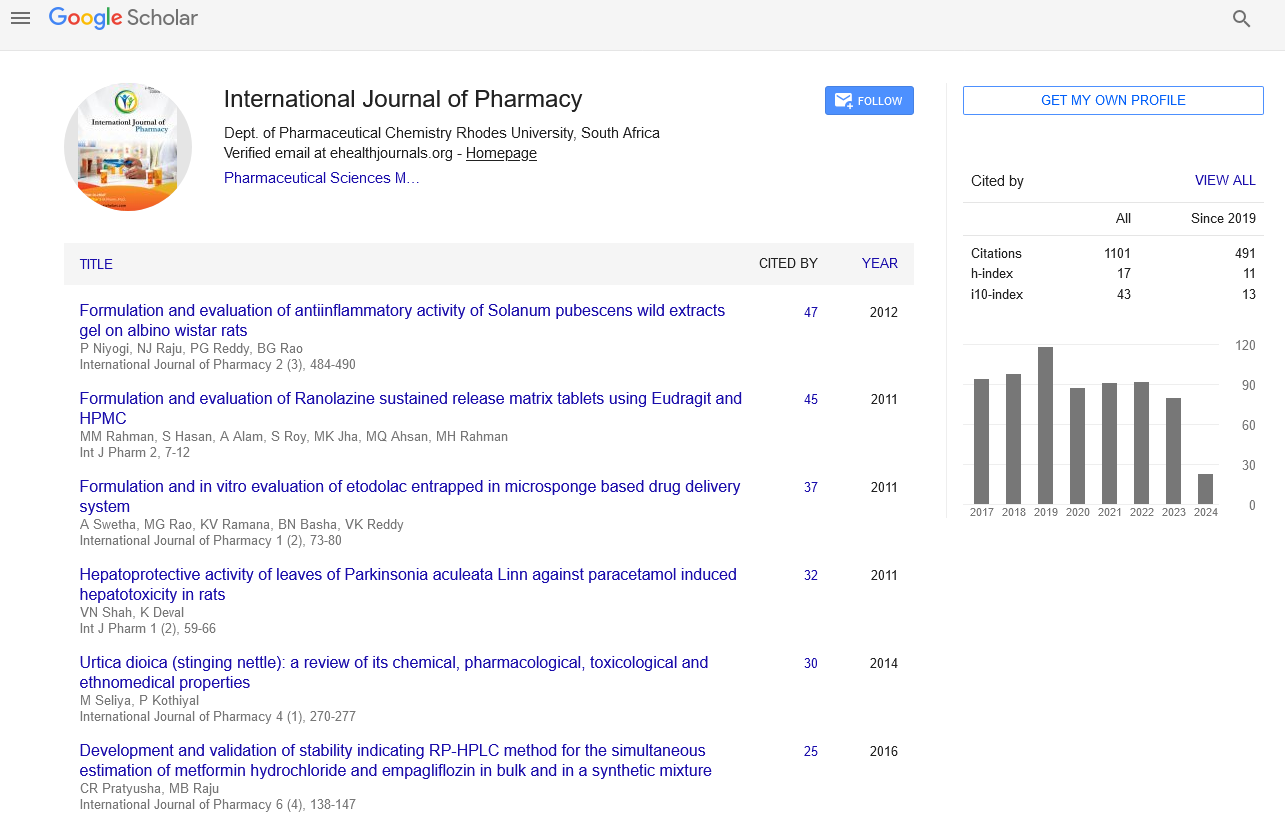
Google scholar citation report
Citations : 1101
International Journal of Pharmacy received 1101 citations as per google scholar report
International Journal of Pharmacy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- HINARI
- Index Copernicus
- Google Scholar
- The Global Impact Factor (GIF)
- Polish Scholarly Bibliography (PBN)
- Cosmos IF
- Open Academic Journals Index (OAJI)
- Directory of Research Journal Indexing (DRJI)
- EBSCO A-Z
- OCLC- WorldCat
- MIAR
- International committee of medical journals editors (ICMJE)
- Scientific Indexing Services (SIS)
- Scientific Journal Impact Factor (SJIF)
- Euro Pub
- Eurasian Scientific Journal Index
- Root indexing
- International Institute of Organized Research
- InfoBase Index
- International Innovative Journal Impact Factor
- J-Gate