HTML
Opinion Article - (2023) Volume 13, Issue 1
Cardiovascular Risk in Patients due to the Effect of Antipsychotic Drugs
Fila Belo**Correspondence: Fila Belo, Department of Analytical Chemistry, University of Lagos, Yaba, Lagos, Nigeria, Email:
Received: 06-Dec-2022, Manuscript No. IJP-22-66796; Editor assigned: 08-Dec-2022, Pre QC No. IJP-22-66796 (PQ); Reviewed: 28-Dec-2022, QC No. IJP-22-66796; Revised: 06-Jan-2023, Manuscript No. IJP-22-66796 (R); Published: 16-Jan-2023, DOI: 10.37532/2249-1848.2023.13(1).27
Description
Patients with schizophrenia are known to have a higher risk of cardiovascular morbidity and mortality. Patients with schizophrenia have a higher risk of sudden mortality than the general population, and are 2-4 times more likely to die young. The cardiovascular adverse effects of Second-Generation Antipsychotics (SGAs) have been linked to catastrophic implications for patients. Because atypical antipsychotics are a chemically varied group of medications, the nature and severity of cardiovascular side effects might vary. Advanced age, autonomic dysfunction, pre-existing cardiovascular disease, female gender (for risk of QTc interval prolongation and torsade de pointes), electrolyte imbalances (particularly hypokalemia and hypomagnesemia), elevated serum antipsychotic drug concentrations, genetic characteristics, and the psychiatric illness itself are all risk factors for cardiovascular adverse effects associated with the use of atypical antipsychotic drugs.
Antipsychotics have been used to treat psychosis for more than five decades. Psychosis can be caused by a variety of conditions, including bipolar disorders, delirium, delusional disorders, psychotic depression, paranoia, schizophrenia, Tourette's syndrome, and substance-induced psychosis, as well as dementias, Huntington's disease, multiple sclerosis, and parkinsonism. The First Generation Antipsychotic Medications (FGAs), also known as "neuroleptics," include phenothiazine, butyrophenones, and thiothixenes, and treat many of the symptoms of psychosis. However, they have undesirable side effects such as akathisia, tardive dyskinesia, dystonia, and Parkinsonism, which are collectively referred to as "Extrapyramidal Side Effects" (EPS). The newer atypical antipsychotics have been found to treat both positive and negative symptoms such as psychosis and apathy and withdrawal, as well as have a positive effect on cognition and a lower risk of EPS.
As previously stated, people with mental illnesses have a higher prevalence of modifiable risk factors for cardiovascular disease, such as obesity, hypertension, diabetes mellitus, and dyslipidemia. Obesity, for example, is 1.5 to 2 times more common among patients with schizophrenia and affective disorders than it is in the general population. According to new research, psychiatric drugs used to treat this population may potentially cause weight gain. A researcher discovered that weight gain increased until 46 weeks after starting clozapine in a five-year naturalistic analysis of people treated with the medicine. Added to additional cardiovascular hazards that mental patients are more prone to, such as sedentary lifestyle, obesity, substance misuse, and smoking, there is obviously a greater rate of cardiovascular mortality related with this demographic. The American psychiatric association's current treatment guidelines indicate that patients with previous heart problems or other cardiovascular hazards be screened for cardiovascular risk before starting antipsychotic therapy and routinely monitored afterward. Wide spectrums of research have indicated a link between SGAs and hypertriglyceridemia. High plasma TG is an independent risk factor for the development of coronary atherosclerosis and coronary heart disease, in addition to age, sex, and low levels of High-Density Lipoproteins (HDL) (CHD). The potential for SGAs to elevate TG is a major issue due to the increased frequency of heart disease and related mortality in the schizophrenic population. The exact mechanism of SGA-induced hyperlipidemia is unknown; however it is more common in people who are overweight or obese. Although all atypical antipsychotics (with the exception of ziprasidone and aripiprazole) elevate serum TG to some extent, clozapine and olanzapine cause severe hypertriglyceridemia. Furthermore, two patients taking quetiapine had a 48 percent increase in TG levels in one short trial. It's worth noting that insulin resistance is suspected to be linked to both hyperlipidemia and hypertriglyceridemia. Hypertriglyceridemia may be linked to decreased islet cell formation and glucose consumption in severe situations (i.e., the development of pancreatitis).
Conclsuion
Antipsychotic drugs have been linked to a variety of cardiovascular problems (e.g., arrhythmias, hypertension, myocarditis, and orthostatic hypotension). Pharmacists and clinicians can better handle and monitor at-risk patients if they are aware of these potential consequences. It's critical to make accurate assessments in order to prevent giving drugs to individuals who don't need them. Regular blood draws and checks of blood pressure, heart rate, respiration rate, and ECG can also assist detect any clinical abnormalities and prevent additional complications.
Manuscript Submission
Submit your manuscript at Online Submission System
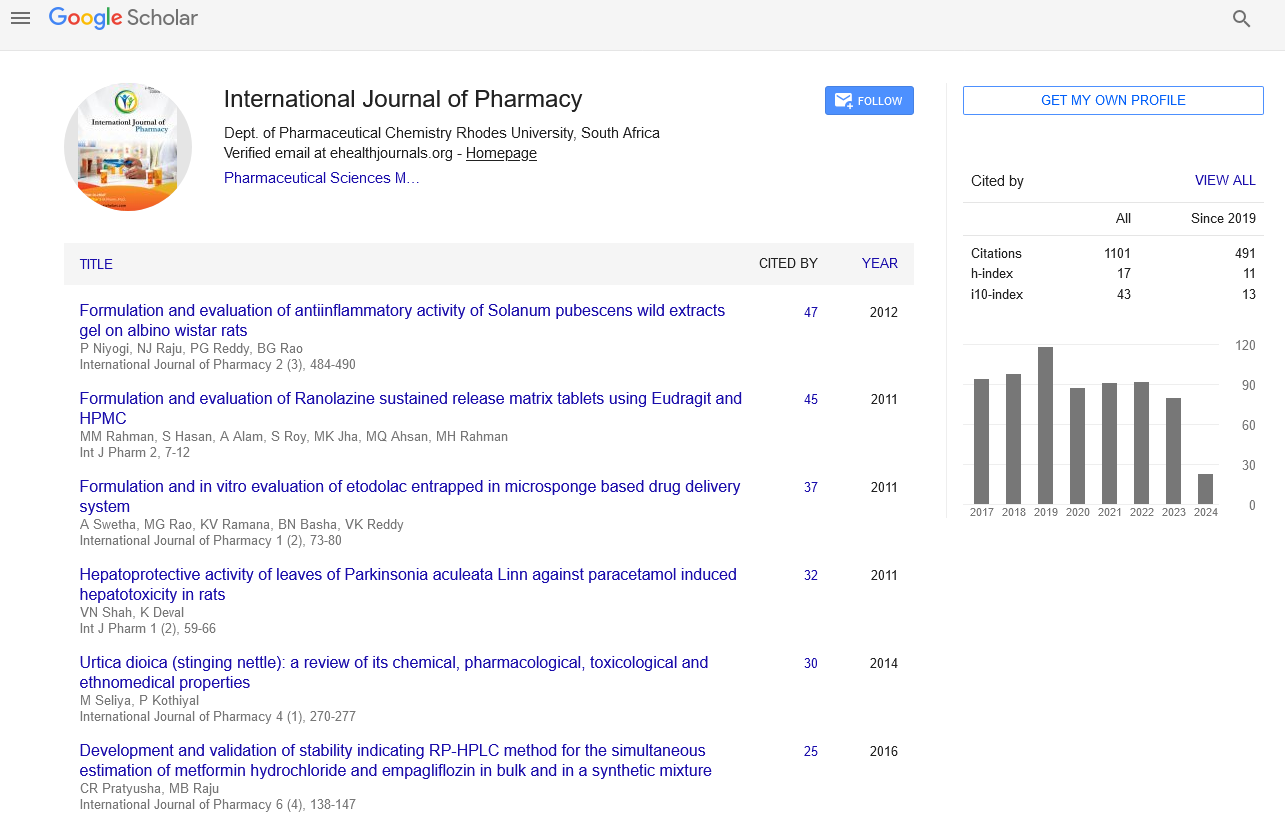
Google scholar citation report
Citations : 1101
International Journal of Pharmacy received 1101 citations as per google scholar report
International Journal of Pharmacy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- HINARI
- Index Copernicus
- Google Scholar
- The Global Impact Factor (GIF)
- Polish Scholarly Bibliography (PBN)
- Cosmos IF
- Open Academic Journals Index (OAJI)
- Directory of Research Journal Indexing (DRJI)
- EBSCO A-Z
- OCLC- WorldCat
- MIAR
- International committee of medical journals editors (ICMJE)
- Scientific Indexing Services (SIS)
- Scientific Journal Impact Factor (SJIF)
- Euro Pub
- Eurasian Scientific Journal Index
- Root indexing
- International Institute of Organized Research
- InfoBase Index
- International Innovative Journal Impact Factor
- J-Gate