HTML
Commentary - (2022) Volume 12, Issue 1
A Short Note on Drug-Interactions of Anticoagulant: Heparin
John Martín**Correspondence: John Martín, Department of Pharmacy, University of Libre de Bruxelles, Brussels, Belgium, Email:
Received: 07-Feb-2022, Manuscript No. IJP-22-150; Editor assigned: 11-Feb-2022, Pre QC No. IJP-22-150 (PQ); Reviewed: 21-Feb-2022, QC No. IJP-22-150; Revised: 28-Feb-2022, Manuscript No. IJP-22-150 (R); Published: 07-Mar-2022, DOI: 10.37532/2249-1848-22.12.01
Description
Heparin is an anticoagulant that prevents blood from clotting. Heparin is a medication that is used to treat and prevent blood clots caused by certain medical diseases or operations. It is also used to lower the risk of blood clots prior to surgery.
Heparin is a prescribed medication that is used to treat and prevent the symptoms of blood clots caused by medical disorders or operations. Heparin can be used alone or in combination with other drugs. Heparin is a medication belongs to a class of drugs Anticoagulants, Cardiovascular, Anticoagulants and Hematologic.
Heparin is a medication that is used to prevent or treat blood vessel, heart, and lung diseases. Heparin is also used to keep blood clots from forming during open-heart surgery, bypass surgery, renal dialysis, and blood transfusions. It is used in low dosages to prevent blood clot development in some patients, particularly those who must have certain types of surgery or who must be in bed for an extended period of time. Heparin may also be used to diagnose and treat disseminated intravascular coagulation, a dangerous blood disorder. This treatment is used to prevent and treat clotting. It has the potential to prevent and cure blood clots in the lungs and legs (including in patients with atrial fibrillation). It may also be used to avoid blood clots during surgery, dialysis, blood transfusions, obtaining blood samples, or when a person is unable to move for an extended period of time. Heparin aids in the smooth flow of blood by improving the function of a naturally occurring molecule in your body (anti-clotting protein).
Heparin may cause serious side effects which includes skin warmth or discoloration, irregular heartbeats, shortness of breath, unusual bleeding or bruising, severe pain or swelling in the stomach, lower back or growing, dark or blue-coloured skin on the hands or feet, nosebleed, skin changes where the medication was injected, purple or red spots under your skin, sudden numbness or weakness, etc.
Heparin Sodium Injectable, USP is a sterile, non-pyrogenic injection solution of heparin sodium (produced from swine intestinal mucosa). Each bottle includes 40 or 80 mg sodium chloride to make it isotonic. The solution contains no bacteriostats, antibacterial agents, or buffers and is solely designed for single-dose injection. When using lesser dosages, the leftover part should be disposed. Heparin Sodium, USP is a heterogeneous group of anticoagulant straight-chain anionic muco polysaccharides known as glycosamino-glycans.
Heparin is very acidic due to the presence of covalently bonded sulphate and carboxylic acid groups. The acidic protons of the sulphate units are partly replaced by sodium ions in heparin sodium. A biological analysis utilising a USP reference standard based on units of heparin activity per milligram is used to measure potency.
Indications
Heparin sodium is used to prevent and treat venous thromboembolism and pulmonary embolism, as well as to treat atrial fibrillation with embolization. Acute and chronic consumptive coagulopathies (disseminated intravascular coagulation) are treated.
Heparin is used in prevention of clotting in arterial and cardiac surgery; prevention and treatment of peripheral arterial embolism; and use of anticoagulants in blood transfusions, extracorporeal circulation, and dialysis treatments.
Drug Interactions
Oral anticoagulants
The one-stage prothrombin time may be prolonged with heparin sodium. When heparin sodium is used with dicumarol or warfarin sodium, blood should be collected at least 5 hours after the last intravenous dosage or 24 hours after the last subcutaneous dose if an acceptable prothrombin time is to be recorded.
Platelet inhibitors
NSAIDS (including salicylic acid, ibuprofen, indomethacin, and celecoxib), dextran, phenylbutazone, thienopyridines, dipyridamole, hydroxychloroquine, glycoprotein IIb/IIIa antagonists (including abciximab, eptifibatide, and tirofiban), and others that inhibit plateletaggregation reactions (the main hemostatic defence) A decrease in the dosage of antiplatelet medication or heparin is indicated to lower the risk of bleeding.
Other interactions
Digitalis, tetracyclines, nicotine, antihistamines, or intravenous nitroglycerin may partially neutralise heparin sodium's anticoagulant activity. Intravenous nitroglycerin administration to heparinized patients may result in a reduction in partial thromboplastin time, with a subsequent rebound effect following nitroglycerin termination. During the coadministration of heparin and intravenous nitroglycerin, it is important to monitor the partial thromboplastin time and modify the heparin dosage.
Antithrombin III (human) in individuals with hereditary antithrombin III deficiency, concomitant therapy with antithrombin III (human) improves the anticoagulant action of heparin. A lower heparin dosage is indicated during antithrombin III therapy to lessen the risk of bleeding (human).
Manuscript Submission
Submit your manuscript at Online Submission System
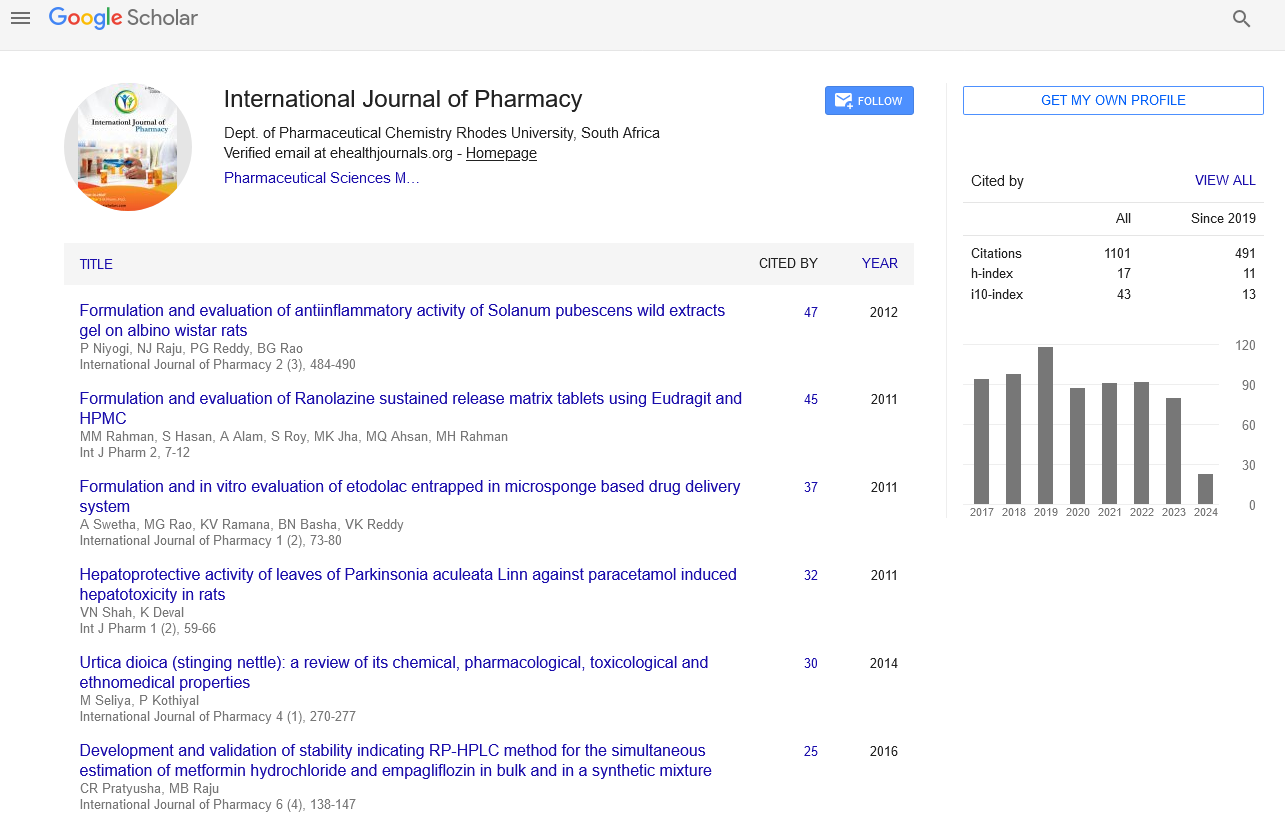
Google scholar citation report
Citations : 1101
International Journal of Pharmacy received 1101 citations as per google scholar report
International Journal of Pharmacy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- HINARI
- Index Copernicus
- Google Scholar
- The Global Impact Factor (GIF)
- Polish Scholarly Bibliography (PBN)
- Cosmos IF
- Open Academic Journals Index (OAJI)
- Directory of Research Journal Indexing (DRJI)
- EBSCO A-Z
- OCLC- WorldCat
- MIAR
- International committee of medical journals editors (ICMJE)
- Scientific Indexing Services (SIS)
- Scientific Journal Impact Factor (SJIF)
- Euro Pub
- Eurasian Scientific Journal Index
- Root indexing
- International Institute of Organized Research
- InfoBase Index
- International Innovative Journal Impact Factor
- J-Gate