HTML
Review Article - (2021) Volume 11, Issue 9
A Review of Depression in Autism Spectrum Disorder (ASD) and a Normal Adolescence
Zaiba Fathima F*, Naveena P, Prabhavathi S and Revathi P*Correspondence: Zaiba Fathima F, Department of Pharmacy, P.S.V College of Pharmaceutical Science and Research, Tamilnadu, India, Email:
Received: 11-Oct-2021 Published: 01-Nov-2021
Abstract
Autism Spectrum Disorder (ASD) is a psychological disorder affected about 1% of the world population (over 75,000,000 people all over the world). Here we discuss the effect of depression and Asperger syndrome with ASD and the effect of depression in the normal adolescence. According to the survey of 2017, people affected by depression globally are 3.4% (approximately about 264 million). Then the World Health Organization (WHO) has recognized depression as the single disease imposing the largest public health burden in the United States and the third largest public health burden in the world. In this review article we discuss the different treatments used according to the patient condition and what are the treatments methods are considered to treat a patient. The diagnosis of depression is difficult in autistic patient when compared with a normal adult and we are observing the case study of few patients and analyse with the help of depression scale. Nearly 8,00,000 people attempts suicide every year which is approximately about a suicide every 40 seconds, suicide is the second leading cause of death for the age group 15-24 years due to depression. Those who suffer from ASD attempts suicide, according to the survey of 2019 studies reporting a range of 7% to 47% attempts suicide and suicide ideation 72% of the cases in small sample. In this review article we are also discuss alternative disorders which come along with depression and ASD. As a result we will be seeing the statistics of the reported cases to reach further conclusions.
Keywords
Anxiety, Behavioural changes, Asperger syndrome, Neurocognitive issues
Abbreviations
CDC: Centre’s for Disease Control and prevention; DSM-5: Diagnostic and Statistical Manual of Mental disorder edition 5
Introduction
Autism Spectrum Disorder (ASD) is characterized both by impairments in social communication and relationships and by the presence of impairing restricted and repetitive patterns of behaviour, interests, or activities. Though some level of impairment must be present before 3 years of age, individuals vary greatly in terms of symptom expression and level of functioning. Up to one half of individuals are functionally nonverbal. Further, a significant proportion of affected individuals have general cognitive and functional abilities consistent with intellectual disability. Repetitive behaviour’s may interfere with learning and activities of daily living.
In addition to these defining symptoms, neurocognitive issues with abstraction and generalization, alexithymia (difficulty identifying feelings) and poor understanding of others' emotions and cognitions (known as theory of mind) are common [1]. Many affected individuals require close supervision to accomplish activities of daily living and/ or maintain safety is commonly, associated medical problems such as epilepsy and bowel dysfunction and psychiatric problems with attention, mood, anxiety, and impulse control increase functional impairment, costs and burden on caregivers.
ASD often impose severe limitations on capacity for managing activities of daily living, and quality of life has been shown to be significantly compromised for many children and families affected by ASD. Studies of comorbid psychiatric illness in ASD indicate high rates of depressive disorders, though they are often under-recognized and likely undertreated. Diagnosis of Major Depressive Disorder (MDD) in the context of ASD can be particularly challenging given atypical presentations of depression in ASD, masking of common depression symptoms by features of ASD, and the lack of standardized diagnostic tools for assessment of depression in those with ASD [2].
Recent studies by the Centres’ for Disease Control and Prevention (CDC) found that 1 in 68, 8-year-old children and 1-91 children of age 3 to 17 years as estimated by the 2007 National Survey of Children's Health had a prior medical or educational diagnosis of ASD. A population-based clinical screening study found that 2.6% of 7 to 12 year olds in Korea were affected, two thirds of whom had not been previously diagnosed. Thus, ASD represents a significant public health concern due to high prevalence, early onset, marked disability and lifelong persistence. The annual prevalence of depressive disorders in the general population is approximately 10%, with rates of 7.5% among adolescents. Depression itself carries an increased risk of medical illness, poor functioning in adolescence and adulthood, and death due to suicide [3].
Due in part to its chronic nature, the World Health Organization has recognized depression as the single disease imposing the largest public health burden in the United States and the third largest public health burden in the world. Depression not only affects the mental health of individuals, but also imposes effects on physical health, which may further contribute to the maintenance of depression. Due both to the high burden of disease and the treatable nature of depression, the US Preventive Services Task Force (USPSTF) has recommended screening all adolescents for depression, provided that a framework for accurate diagnosis, treatment and follow-up is in place. Prevalence of suicide attempts varied between 7% and 47%, while suicidal ideation was reported in up to 72% of cases. Being male and having a history of selfharm and depressions were cited as significant risk factors. Suicidal attempts and ideations are increased in ASD; however, the extent of the increase and the risk factors identified within this group remain underinvestigated [4].
Literature Review
The new Diagnostic and Statistical Manual of Mental Disorders, Edition 5 (DSM-5), proposes Autism Spectrum Disorder (ASD) as the only diagnosis possible for the previous category of pervasive developmental disorder, as well as the elimination of Asperger Syndrome (AS). This change in name emphasizes the dimensional consideration of the clinical picture in the various areas affected (social communication and mental inflexibility) and the difficulty of establishing precise limits between the subgroups within the same category. This new classification is based on empirical evidence that the majority of individuals with a diagnosis of AS meet the DSM-IV criteria for Autistic Disorder [5-8].
In addition, there is a consensus as to the need to go deeper in reconsidering not only diagnostic issues, but also co morbidity, assessment, and intervention in ASD. Individuals with ASD show significant variability in symptom expression and in the level of cognitive functioning (DSM-5). In addition, their condition can coexist with other disorders. The studies that confirm the high risk of co morbidity with depression are notable. Fundamentally, in adolescence, individuals with High Functioning Autism Spectrum Disorders (HFASD) usually present a high degree of anxiety, stress and depression, with mood disorders being the most common co morbidity. However, because the main symptoms of ASD cause significant impairment, other psychopathological symptoms are usually not the primary focus of screening, diagnosis, or treatment. Research suggests that such conditions can exacerbate the core ASD symptoms, compromising quality of life and long-term functioning level even more. That is why there is a need for specialized attention to prevent the possible appearance of depressive symptomatology, for early detection and for specific intervention if depression has appeared. The work of experts in early detection and intervention becomes more difficult [9-11].
Attempting to enhance professional praxis in prevention, early detection and early intervention, we consequently propose the following;
• Presenting the rates of depression in children and adolescents with HFASD.
• Analysing the possible risk factors and explicative hypotheses for diagnostic and/or symptomatological co-morbidity of HFASD and depression, establishing a possible working hypothesis that supports studying the profiles of potential vulnerability and contributing factors.
• Assessing the implications of depression in HFASD (the risk of suicide).
• Analysing the difficulties involved in assessing depression in children and adolescents with HFASD and proposing alternatives. All of these would make it possible to elaborate a proposal, in agreement with the results obtained from these analyses, that promotes and establishes possible future research paths, which would complement, refute, or confirm the studies carried out to date [12].
There are six different psychotherapies for depression;
• Cognitive therapy
• Behavioural therapy
• Cognitive behavioural therapy
• Dialectical behavioural therapy
• Psychodynamic therapy
• Interpersonal therapy
They use different approaches for therapy like individual therapy, family therapy, group therapy, couple therapy [13].
Methodology
Participants were assessed at the Washington University, Autism Centre as part of the NIMH STAART Centre of Excellence Study or the NICHD CPEA Family Study of Autism (U54MH066399N or U19HD34565, Geraldine Dawson, PI). Potential participants were excluded for having identifiable genetic disorders associated with autism (fragile X syndrome, Norrie syndrome, neurofibromatosis, tuberous sclerosis), sensory or motor impairment, seizures, cerebral palsy, major physical abnormalities, current psychoactive medications or inability to undergo an MRI (as part of another study). Forty-six adults with ASD, ranging in age from 18 to 44 years (M=23.70, SD=7.21), participated. Participant self-report of race and ethnicity yielded the following information: 44 Non-Hispanic or White, one African American, one more than one race. After complete description of the study, written informed consent was obtained. Clinicians administering the measures were blind with respect to the hypothesis being tested in this study. All participants were diagnosed with an autism spectrum disorder using a parent interview, the Autism Diagnostic Interview-Revised (ADI-R), which uses criteria for autism according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSMIV; APA 1994) and the Autism Diagnostic Observation Schedule (ADOS), a semi-structured observation and interview administered directly to the participant. Participants interviewed as part of the NIMH STAART Centre of Excellence Study (n=37) were given the WPS version of the ADOS (ADOS-WPS), and the 9 participants interviewed as part of the NICHD CPEA Family Study of Autism were administered the Generic version of the ADOS (ADOS-G). The subset of items being compared on the ADOS in the current study did not differ between the two versions [14]. The ADOS yields a total score as well as separate communication and social domain scores. The communication domain measures symptoms related to verbal and nonverbal communication (e.g., speech abnormalities, stereotypic speech, gestures), while the social domain measures symptoms related to empathy, insight, social reciprocity, use of social overtures, and social response to others. All participants in the current study were administered Module 4 of the ADOS, given their ability to use fluent speech. Inter-rater reliability was assessed by double coding a subset of the sample using procedures outlined by Shrout and Fleiss; intra-class correlations were 88 or higher on all ADOS and ADI subscales. IQ was estimated using four subtests of the Wechsler Adult Intelligence Scale-Third Edition (WAISIII): vocabulary, comprehension, block design, and object assembly. Psychiatric symptoms were assessed using a standardized psychiatric history interview. The University of Washington research team adapted a Family History Interview developed by Rutter and Folstein, by adding Research Diagnostic Criteria (FH RDC) for psychiatric conditions not originally included in the interview, including depression, manicdepressive disorder, anxiety disorders, Obsessive Compulsive Disorder (OCD), drug and alcohol abuse, conduct disorders, and psychosis. Specific probes for each interview item, as well as criteria used for coding each item, were based on DSM-IV (APA 1994) definitions. A trained clinician administered the 15-30 min interview with each participant. Clinicians evaluated the participant’s depressive symptoms, including feelings of misery, loss of interest, sleep and appetite disturbance, and feelings of self-blame and hopelessness, as well as associated impairment and/or history of professional treatment for depression. Based on self-report of symptoms, clinicians assigned the participant to one of the following categories of depression: (a) None (no depressive symptoms; n=26); (b) Probable but insufficient information to meet criteria for more severe levels of depression (n=4); (c) Definite disorder, including at least one month of unhappiness, anhedonia and social impairment or treatment (social impairment includes missing school or having decreased performance at school or other activities, or decrease in socialization; n=14); (d) Hospitalized for at least 2 days or Electro-Convulsive Therapy (ECT) before age 16 (n=1); or (e) Definite episode of at least 2 weeks, but less than 1 month (n=1). Participants in categories 2 through 5, endorsing symptoms of depression, were collapsed into the ‘depressed’ group. This group consisted of 20 individuals (43% of the participants). The ‘nondepressed’ group consisted of the 26 individuals who did not endorse any symptoms related to depression [15].
Table 1 presents the gender and ages of both groups. The two groups differed significantly on age, t (44)=@2.76, p\01, such that on average, the depressed group contained older individuals. Symptoms related to general anxiety and OCD were assessed according to a similar system, described in more detail below. The number of participants in each group (depressed and non-depressed) endorsing symptoms related to anxiety and OCD are presented in Table 2. To evaluate general anxiety, participants were asked about their overall level of fear, anxiety, and worry, in addition to experiences of agoraphobia and panic attacks. Categories included: (a) None; (b) Probable, but insufficient information to meet criteria for more severe anxiety; (c) Chronic or recurrent severe anxiety, agoraphobia or panic, with at least one clear example of observable behaviour’s (e.g., staying at home, reassurance seeking, trembling, pacing, treatment); (d) Hospitalized for at least 2 days or ECT before age 16; or (e) Sub-threshold level of symptoms (significant but not definite symptoms). In order to evaluate symptoms related to OCD, participants were asked whether they have specific rituals or routines he or she needs to carry out, or thoughts that he or she cannot get out of mind that are inappropriate or disturbing. Categories for self-report of OCD related symptoms included: (a) None; (b) Probable but insufficient information to meet criteria for more severe OCD; (c) Definite symptoms; (d) Sub-threshold level of symptoms (Tables 1 and 2).
| Gender | Depressed (n=20) | Non depressed (n=26) |
|---|---|---|
| Male | 19 | 23 |
| Female | 1 | 3 |
| Mean(SD) | 26.82(8.76) | 21.30(4.62) |
| Range | 18.33-44.75 | 18.00-35.08 |
| Endorsing symptoms | Depressed (n=20) | Non depressed ( n=26) |
|---|---|---|
| Anxiety disorder total | 9 | 4 |
| None | 11 | 22 |
| Probable | 3 | 0 |
| Chronic or recurrent severe anxiety | 5 | 2 |
| Hospitalized at least 2 days or ECT | 1 | 0 |
| Sub-threshold level of systems | 0 | 2 |
| Obsessive compulsive disorder total | 11 | 5 |
| None | 9 | 21 |
| Probable | 5 | 3 |
| Definite | 4 | 0 |
| Sub threshold, significant but not definite | 2 | 2 |
| Endorsing both anxiety and OCD symptoms | 4 | 1 |
Autism Diagnostic Observation Schedule Analysis
To assess whether the depressed and non-depressed groups differed in terms of cognitive ability, independent samples t-tests were conducted, comparing full scale, performance and verbal WAIS scores by group. Independent samples t-tests revealed significant cognitive differences between groups, such that on average, individuals who endorsed symptoms of depression had significantly higher overall full scale cognitive scores and significantly higher verbal abilities as estimated by the WAIS. Although the depressed group also showed a trend toward higher performance IQ scores, this difference was not significant. The results suggest that in this sample, individuals endorsing symptoms of depression had higher levels of cognitive ability, with IQs in the average to above average range [16].
Finally, to determine whether the presence of other psychiatric symptoms was associated with higher levels of depressive symptoms, we examined the percentage of anxiety and obsessive–compulsive related symptoms for the depressed and non-depressed groups. Almost half (45%) of the individuals endorsing depressive symptoms also endorsed symptoms related to general anxiety, whereas only 15% of the non-depressed group endorsed such symptoms [17,18].
Depression scale
The Centre for Epidemiologic Studies Depression Scale (CES-D Scale) was developed for use in studies of the epidemiology of depressive symptomatology in the general population. Its purpose differs from previous depression scales which have been used chiefly for diagnosis at clinical intake and/or evaluation of severity of illness over the course of treatment. The CES-D was designed to measure current level of depressive symptomatology, with emphasis on the affective component, depressed mood. The symptoms are among those on which a diagnosis of clinical depression is based but which may also accompany other diagnoses to some degree.
Evidence that the scale is reliable but are also sensitive to current levels of symptomatology will be based on predictability of test-retest changes in scores (e.g., scores of patients before and after treatment or scores of household respondents before and after “Life Events Losses”).
The CES-D was designed for use in general population surveys, and is therefore a short, structured self-report measure. The scale was designed for use in studies of the relationships between depression and other variables across population subgroups. To compare results from one subgroup to another, the scale must be shown to measure the same thing in both groups (Table 3).
| S.NO. | List of ways you might have felt or behaved | During the past week | |||
|---|---|---|---|---|---|
| Rarely or none of the time (less than day) | Some or little of the time (1-2 days) | Occasionally or moderate amount of time (3-4 days) | All of the time (5-7 days) | ||
| 1 | Was bothered by things that usually don't bother me | 0 | 1 | 2 | 3 |
| 2 | Did not feel like eating: My appetite was poor | 0 | 1 | 2 | 3 |
| 2 | Felt that could not shake off the blues even with help from my family or friends | 0 | 1 | 2 | 3 |
| 4 | I felt was just as good as other people | 0 | 1 | 2 | 3 |
| 5 | I had trouble keeping my mind on what was doing | 0 | 1 | 2 | 3 |
| 6 | Felt depressed | 0 | 1 | 2 | 3 |
| 7 | Felt that everything did was an effort | 0 | 1 | 2 | 3 |
| 8 | Felt hopeful about the future | 0 | 1 | 2 | 3 |
| 9 | Thought my life had been a failure | 0 | 1 | 2 | 3 |
| 10 | Felt fearful | 0 | 1 | 2 | 3 |
| 11 | My sleep was restless | 0 | 1 | 2 | 3 |
| 12 | Was happy | 0 | 1 | 2 | 3 |
| 13 | Talked less than usual | 0 | 1 | 2 | 3 |
| 14 | I felt lonely | 0 | 1 | 2 | 3 |
| 15 | People were unfriendly | 0 | 1 | 2 | 3 |
| 16 | Enjoyed life | 0 | 1 | 2 | 3 |
| 17 | Had crying spells | 0 | 1 | 2 | 3 |
| 18 | Felt sad | 0 | 1 | 2 | 3 |
| 19 | Felt that people dislike me | 0 | 1 | 2 | 3 |
| 20 | Could not get "going" | 0 | 1 | 2 | 3 |
Presentation of depression in ASD
Two case vignettes are presented below, to highlight the key challenges in diagnosing co-morbid depression in ASD. The first involves a verbal young adult. The second involves the minimal verbal school-aged child [19].
Case 1 Jack: Jack had been diagnosed with ASD at 30 months of age and developed phrase speech at 8 years of age. He was particularly interested in popular music and physical fitness, interacted around these interests with family and adults in the neighbourhood, and was very insistent on following his routines, but had never been aggressive. Nine months before he came to the clinic, he had graduated from high school at age 22 and had begun working with a job coach at a local grocery store. His younger brother had also graduated and moved away to college. Things went well for the first few months, but then he began to have difficulty sleeping and was eating less. He began exercising for more extended periods and complained to his parents that his muscles were melting. He began to check his appearance in mirrors so frequently that it interfered with his daily activities. At the same time, he was more withdrawn and seldom talked with the neighbours any more. He was in almost constant motion, pacing, playing basketball or walking the dog. He also was more irritable and on occasion pushed furniture over when he felt others were interfering with his activities. On mental status exam, he spoke very little and often seemed preoccupied or confused. When asked about his mood he said “not good” and talked about his muscles. He said there was a black shadow coming over his arms and legs and he was not himself. His affect was irritable especially when asked direct questions. He denied any desire to hurt himself or others. He did not respond to questions about the duration of his problems, things that he enjoyed, or things that may have been upsetting. His parents were primarily concerned about his withdrawal, irritability and agitation. Family history was positive for schizophrenia, depression, and severe anxiety. His parents were reluctant to try an antipsychotic medication and he was started on fluoxetine. Within 3 months he was sleeping better, and was less physically agitated and less irritable. He no longer looked in the mirror or talked about his muscles. However, he remained more withdrawn than his baseline for 4 more months despite increases in his fluoxetine. After 1 year, his family and he felt he was back to his usual self.
Case 2 Philip: “Philip” was 16 years old and had diagnoses of ASD and severe ID. He had limited verbal language skills but asked for familiar objects and different kinds of food using single or two word utterances. Philip also displayed extensive echolalia, repeating phrases which were challenging to connect to the current situation. Philip was referred to a specialized psychiatric inpatient unit for adults with ASD/ ID for re-assessment due to several unsuccessful treatment attempts of his severe SIB.
Philip is the oldest child of unrelated parents. Philip was diagnosed with ASD and unspecified ID when he was 4. The latter diagnosis was later changed to moderate ID, and again to severe ID when Philip was 14. The births of his two younger siblings and his behaviour becoming increasingly challenging for his parents to manage resulted in Philip spending increasing periods of time in a care home during his schoolage years. Philip moved into full-time care when he was 10 and into a new care home at 14. He received frequent visits from his family in both homes.
At referral, Philip on average had 20-30 daily episodes involving severe head banging against walls or the floor. Attempts to interrupt these episodes by professional caregivers usually led to aggression, including Philip attempting to kick, bite or hit caregivers. Both Philip himself and several caregivers had sustained physical injuries during such episodes. Due to the severity of episodes and caregivers lacking other options to limit physical injury, at the time of the referral SIB was managed by two to three caregivers manually restricting Philip face down on the floor on a rubber mat until episodes subsided.
Philip’s SIB had developed gradually, starting in his preschool years with frequent wrist biting and Philip occasionally hitting his face with his fist. When Philip was about 13 years old, he had an episode of passivity and social withdrawal where he refused to go to school or leave his room, lost weight and seemed generally unhappy. During this episode, his professional caregivers targeted these behaviour’s as passivity, working systematically to increase Philip’s compliance to everyday demands. These interventions increased his participation in basic tasks such as hygiene, mealtimes and going to school, but it was also during this period that Philip’s SIB became more severe and he started banging his head against hard surfaces. At referral, episodes of SIB had reached a level of severity that limited Philip’s activities and he mostly stayed inside his apartment.
Several previous attempts had been made to reduce Philip’s SIB. These attempts had included varying strategies from applied behaviour analysis. Reinforcement-based strategies had been attempted initially, with subsequent attempts including overcorrection and punishmentbased strategies. In spite of this, Philip’s SIB had gradually worsened in frequency and intensity. No previous psychiatric assessment had been conducted. Pharmacological interventions had been attempted, including use of antipsychotics, benzodiazepines and antiepileptic’s, but none of these attempts resulted in any lasting change to the frequency or intensity of Philip’s SIB. At referral Philip received 30 mg. of alimemazine for sleep.
Case 3 Rican: The patient was a 15 year old Puerto Rican adolescent female living with both her parents and a younger sibling. Her parents presented with significant marital problems had been separated several times and were discussing divorce. Her mother reported having a history of psychiatric treatment for depression and anxiety and indicated that the patient's father suffered from bipolar disorder and had been receiving psychiatric treatment. He was hospitalized on multiple occasions during previous years for serious psychiatric symptoms.
The patient was failing several classes in school and her family was in the process of looking for a new school due to her failing grades and difficulties getting along with her classmates. She presented the following symptoms: frequent sadness and crying, increased appetite and overeating, guilt, low self-concept, anxiety, irritability, insomnia, hopelessness, and difficulty concentrating. In addition, she presented difficulties in her interpersonal relationships, persistent negative thoughts about her appearance and scholastic abilities, as well as guilt regarding her parents' marital problems.
The patient's medical history revealed that she suffered from asthma, used eyeglasses, and was overweight. Her mother reported that she had been previously diagnosed with MDD 3 years ago and was treated intermittently for 2 years with supportive psychotherapy and anti-depressants (fluoxetine and sertraline; no dosage information available). This first episode was triggered by rejection by a boy for whom she had romantic feelings. Her most recent episode appeared to be related to her parents' marital problems and to academic and social difficulties at school.
Discussion
Autistic treatment questio nnaires
The original questionnaire included;
• Personal demographics
• Treatments used
• Factors related to treatment choice
• Beliefs about the treatment effectiveness, causes described behavioural changes
• Rating for treatment effectiveness according to population specificity
• Treatment where defined within the questionnaire to provide participants with a clear indication of the treatment involved. See Table 3 for induced treatment categorized according to support level. Participants indicate (yes/no) weather the perceived each treatment to be effective for the following population;
• People with Intellectual or Developmental Disabilities (IDD)
• People with ASD
• People with severe behavioural problem
• Adults children,
• All people
• No one
ASD patient may meet the therapist for 25 hours per week for floor time studies show that most children who have floor time therapy for 25 hours a week for 2 years or longer improve in all areas of development (Table 4).
| Established | Emerging | Un-established | Ineffective/harmful |
|---|---|---|---|
| Applied behavior analysis | Music therapy | Sensory integration | Chelation therapy |
| Positive behavioral | Floor time | Son-rise | Gluten and casein free diet |
| Discrete trial instruction | Picture exchange communication system | Applied verbal behavior | Vitamin therapy |
| - | TEACCH | Craniosacral therapy | Holding therapy |
| - | - | Faith-based therapy | Hyperbaric oxygen |
| - | - | Speech therapy | Auditory integration |
| - | - | Chiropractic | Facilitated communication/rapid prompting |
Treatment given to Rican (only depression)
The patient was treated using a manual-based CBT, which has demonstrated success in treating depression in Puerto Rican adolescents. She participated in a research project on therapy for depression in adolescents, which compared a standard 12-session “dose” of CBT only, with CBT enhanced with a group psycho-educational 8-session parent intervention. She was randomized into the CBT only condition of the study. As part of a supplemental research project, additional sessions (up to a maximum of 12) were offered to adolescents whose depression did not remit at post treatment to examine the optimal dose needed for complete remission as well as characteristics associated with treatment response. Five adolescents agreed to participate in this study and received an average of seven additional sessions. The adolescent chosen for the case study had a therapist who was a doctoral level graduate student in clinical psychology trained in CBT who received weekly supervision from a licensed clinical psychologist with a PhD. Qualitative data for this case study were analyzed by reviewing progress notes and video recordings of therapy sessions.
Sessions (1-4): The first four sessions focused on teaching the patient about the influence of thoughts on mood and strategies to debate dysfunctional thought patterns and increase positive thoughts. During the week, the patient was asked to complete a daily mood thermometer, which was discussed at the beginning of every session. Homework assignments such as keeping a daily log of positive and negative thoughts and identifying and challenging dysfunctional thoughts were some of the homework assignments that the patient completed between sessions.
The patient's mood fluctuated widely during these first sessions. She cried several times and verbalized feelings of sadness, guilt, and low self-concept. The main dysfunctional thoughts identified and challenged during these sessions were mostly about herself (I'm ugly and stupid; People look at me because I'm fat), anxiety over not being able to fit in at a new school (I won't know anyone; I'll be far away from my friends; It'll be too hard), and guilt about her parents' marital problems (My parents fight because of me; If I had better grades they wouldn't fight). By the fourth session, she succeeded in rationally challenging several of these negative thoughts (I can make new friends; I have a chance to start over at a new school; I am good at drawing and I have a good sense of humour). Nonetheless, many negative thoughts persisted, mostly surrounding her parents' relationship. By the end of this therapy module, the patient began to share some of her artistic talents with the therapist and her self-concept appeared to be improving.
Sessions (5-8): The following four sessions worked with increasing pleasant activities, time management, and goal setting to improve mood. Homework assignments in this module involved keeping a daily log of pleasant activities, completing a weekly planner, and establishing specific goals and steps to complete them.
By the 5th session, the patient's mood improved significantly, most likely due to having a positive experience at her new school; she had made new friends, her grades had improved, and she was getting along well with her teachers. She also reported a decrease in depressive symptoms. This positive experience at school was used in therapy to help the patient challenge negative thoughts and expectations by providing evidence that disqualified them (i.e. she is likeable, she can cope in a new school). Consequently, the number of negative thoughts she had decreased markedly, and this reduction was reinforced verbally by the therapist.
The patient recognized that one of the barriers to enjoying pleasant activities, particularly social activities, was her negative thoughts (I'll make a fool of myself; I won't do it right; I'll be rejected by others) and her parents (obtaining permission for certain activities). The patient kept track of her pleasant activities and began to organize her time better to accommodate her homework and chores by using a weekly planner. This allowed the patient and therapist to evaluate whether she had an adequate balance of pleasant activities in her schedule that helped improve her mood and make adjustments accordingly. Role-playing exercises were used to help the patient learn to negotiate permission from her parents to participate in social activities. Her self-concept continued to improve as evidenced by her verbalizations (Sometimes I feel pretty) and her physical appearance (increased confidence, better posture, and grooming). The therapist reflected these observations back to the patient. She was also handling stressful situations better as evidenced by her reaction to being teased at school; she simply ignored it instead of feeling sad and having persistent negative thoughts about herself, which would have typically been her response. This suggests that the patient was internalizing skills learned in the first few sessions, such as thought-stopping techniques to decrease negative rumination.
Sessions (9-12): The last four sessions worked on the ways in which interpersonal relationships affect mood and focused on increasing and maintaining social support, as well as improving assertive communication skills. The patient reported having a good social support system, but complained about one of her close friends who would often put her down; this would activate negative thoughts about her abilities and attractiveness. This relationship was examined in the context of adequate expectations for friendships. The patient presented a passive communication style, which was contributing to feeling hurt frequently and having her emotional needs unmet. Thus, the focus of two sessions was to work on developing assertiveness through roleplaying exercises. She reported some upsetting incidents at school between her new and old friends but appeared to be handling them well using cognitive strategies learned in the first module.
However, during the last few sessions of this module the patient was still experiencing feelings of guilt, anger, and sadness about her parents' marital problems. Notably, she was disturbed by significant communication problems between her parents who often spoke negatively about one another in her presence and used her as a messenger to communicate with each other. She confided in the therapist about having witnessed physical and emotional abuse between her parents, as well as living through several separations over the previous 10 years. The therapist explored the possibility of having a session with her parents to discuss how their problems affected the patient, and she agreed. During this session the therapist discussed with the parents how their behaviour was contributing to the patient's depressive symptoms and recommended marital therapy. The parents admitted to having significant problems and agreed to seek couples therapy.
Additional sessions (13-16): On completion of the standard 12-session “dose” of CBT, the patient was still presenting symptoms of depression in the severe range and continued to meet criteria for MDD; hence, she received additional sessions of CBT until her symptoms decreased and she no longer met MDD criteria according to the DISC-IV, as established by the study's protocol for additional sessions. These four sessions worked mostly with the patient's feelings and thoughts surrounding the possibility of her parents' divorce or separation. The focus was on how to manage these feelings in order to decrease their impact on her mood and daily functioning.
The patient's main negative thoughts were mostly related to fear that her father would leave and never contact her, and that he would remarry and have another family with whom she might not get along. These were challenged in therapy by asking the patient to find evidence that these thoughts would actually come true. The patient realized that most of her friends whose parents had divorced had good relationships with them and their new families, and acknowledged that although her father had often threatened to leave, he had also told her that he would always be there for her. She also realized that it was possible that things would be better if they separated and that their fights might even decrease. In addition, role-playing exercises were used to practice talking to her father about her fears and worries regarding the possibility of his leaving and how it would affect their relationship.
On termination, the patient's depressive symptoms were in the moderate range and she no longer met criteria for MDD according to the DISCIV, which was one of the study's criteria for ending therapy. In addition, her self-concept had improved, and the therapist observed decreased dysfunctional attitudes and suicidal ideation. These improvements were maintained at 6 and 12-month follow-up assessments, and her depressive symptoms decreased to mild by the last three follow-up assessments [20].
During the last session, the therapist worked on closure with the patient, reinforced improvements in the patient's mood and coping skills, and counselled the patient on relapse prevention strategies. Relapse prevention strategies include monitoring depressive symptoms and recognizing the need for treatment if they worsen or recur, and using cognitive-behavioural strategies to manage her mood (i.e. debating dysfunctional thoughts, planning pleasant activities). The therapist also counselled the patient's mother on how to monitor her daughter's residual symptoms and the importance of seeking treatment if symptoms worsened. She also reiterated her previous recommendation that the parents seek couples counselling, which they had yet to do.
The left column lists characteristics of depression seen in both children and adults. The asterisks (*) indicate qualities that are unique to or more commonly observed in childhood depression. The presentation of depression in children with autism spectrum disorders can be more challenging to characterize and recognize. The right column lists additional characteristics that have been described in ASDaffected children presumed to be affected by depression or depressive symptomatology (ASD-affected children have been observed to exhibit signs or symptoms from both the left and right columns) (Table 5).
| Traditional signs and symptoms of depression including characteristics that may be seen in childhood depression | Additional signs and symptoms that may be present in ASD-affected children who are experiencing depression |
|---|---|
| Depressed mood, sadness, tearfulness | Aggression |
| Irritability* | Mood liability |
| Anhedonia | Hyperactivity |
| Insomnia or hypersomnia | Decreased adaptive functioning or self-care |
| Psychomotor agitation or retardation (behavioral problems*) | Regression of previously learned skills |
| Fatigue or loss of energy | Increased compulsiveness |
| Social withdrawal | Fluctuations in autistic symptoms including both increased stereotypic behavior and decreased interest in preoccupations/restricted interests |
| Weight loss not associated with dieting / change in appetite | Self-injurious behavior |
| Increased guilt or worthlessness | Catatonia |
| Somatic complaints* | Overall marked change in behavior from baseline not otherwise specified by above characteristics |
| Lack of brightening* | - |
| Diminished ability to concentrate; indecisiveness | - |
| Recurrent thoughts of death or suicidal ideation | - |
| Play characterized by themes of suicide or death* | - |
Note: The asterisks (*) indicate qualities that are unique to or more commonly observed in childhood depression.
Conclusion
study shows that the diagnosis of the depression is not easy in ASD. Autistic people are four times as likely to experience depression over the course of their lives as their neurotypical peers, 40 percent of adults with ASD experience depression at some point during their lifetime. The most commonly prescribed antidepressant drugs used to treat depression in ASD are fluoxetine and sertraline it may differ according to the patient condition or severity.
A person with Asperger’s becomes depressed not due to life stress related to autism symptoms, but it may occur due to direct factors that cause depression. Treatment strategies are with a team of professionals to meet the needs of a patient, for managing other medicinal and mental health conditions. Many studies indicate preliminary efficacy for Mindfulness Based Therapy (MBT) and others explained the effect of Cognitive Behavioural Therapy (CBT), having 6-8 sessions offers more benefit than 1-5 sessions, however the results are inconsistent. Although it is possible that depression is underestimated, especially is the contest of ASD.
Consent
Patient confidentiality has been maintained and written consent for the publication of patient details.
References
- Chandrashekar T, Sikich L. Int. med. Nat. Inst. Health. 2015; 17(2): 219-227.
- Arlington V. Ind. J. Psy. 2013; 55(3): 220-223.
- Leyfer OT, Folstein SE, Bacalman S. J. Autism. Dev. Disord. 2006; 36: 849-861.
- Chen CY, Chen KH, Liu CY, Huang SL, Lin KM. J. Pediatr. 2009; 154(3): 345-350.
- Matson JL, Schwalm NMS. J. Res. Dev. Disabil. 2007; 28: 341-352.
- Cidav Z, Lawer L, Marcus SC, Mandell DS. J. Autism. Dev. Disord. 2013; 43(4): 924-931.
- Katherine M, Magnuson BS, John N, Constantino MD. J. Dev. Beh. Pediatr. 2011; 32(4): 332-340.
- Zahid S, Rachel U, J. Int. Suic. Prev. 2017; 38(4): 237-246.
- De-la-Iglesia M, Olivar J. J. Sci. World. 2015.
- Stewart ME, Barnard L, Pearson J, Hasan R. J. Sage. 2006; 10(1).
- Montgomery SA, Asberg M. Brit. J. Psy. 1979; 134(4): 382-389.
- Kildahl AK, Bakken TL, Matre EAW, Hellerud JMA, Engebretsen MH, Helverschou SB. Int. J. Dev. Disab. 2021; 67(5): 327-338.
- Chafey MIJ, Bernal G, Rossello J, J. Depres. Anxi. 2009; 26(1): 98-103.
- Clarke GN, Rohde P, Lewinsohn PM, Hops H, Seeley JR. J. Amer. Acad. Child. Adolesc. Psy. 1999; 38(3): 272-279.
- March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, Burns B, Domino M, McNulty S, Vitiello B. JAMA. 2004; 292(7): 807-820.
- Happe F, Frith U. J. Neuro. psy. Autism. 1996; 119(4): 1377-1400.
- Spencer D, Marshall J, Post B. J. Pediatrics. 2013; 132(5): 833-840.
- Boerma J, Fat DM, Mathers C. WHO. 2008.
- Miller KD, Hammen CL, Brennan PA. J. Adolesc. Health. 2007; 41(3): 256-262.
- Humphey N, Lewis S. J. Sage. 2008; 12(1): 23-46.
Manuscript Submission
Submit your manuscript at Online Submission System
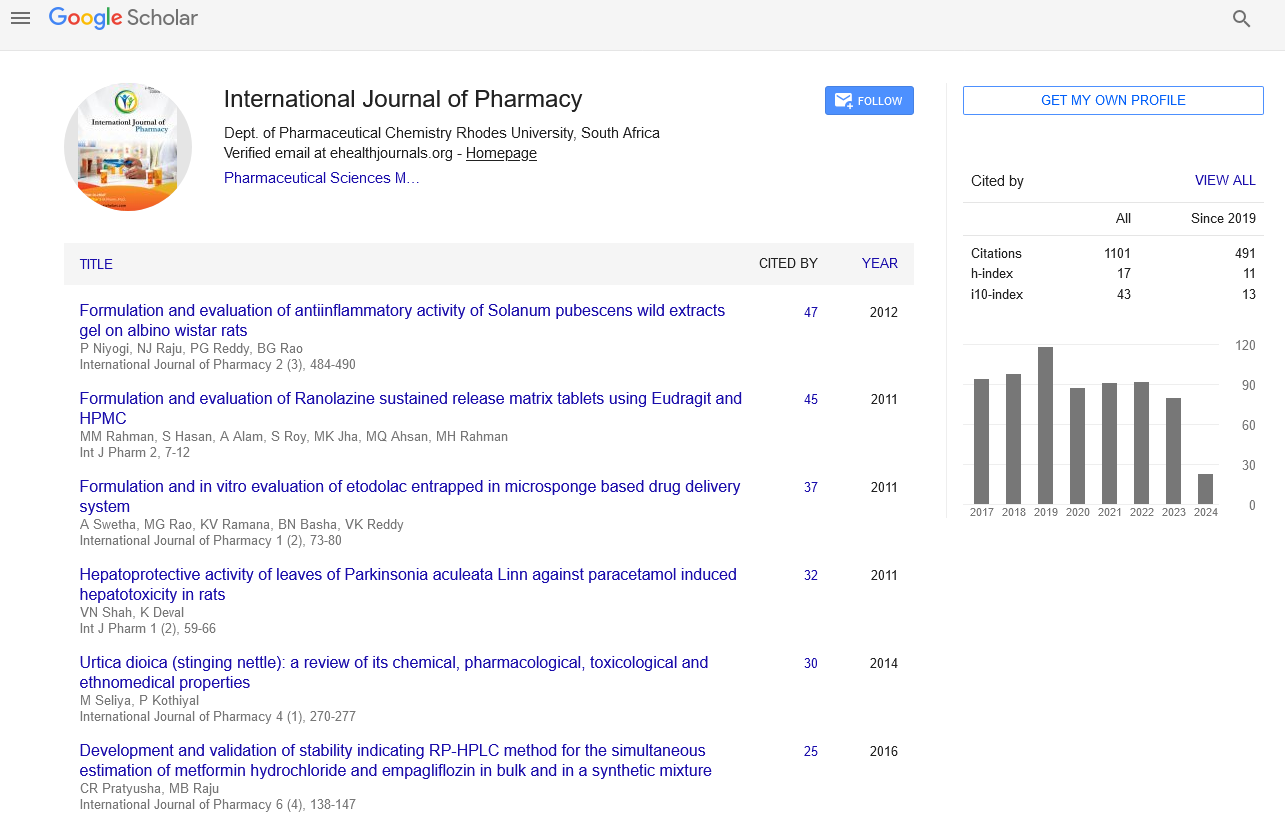
Google scholar citation report
Citations : 1101
International Journal of Pharmacy received 1101 citations as per google scholar report
International Journal of Pharmacy peer review process verified at publons
Indexed In
- CAS Source Index (CASSI)
- HINARI
- Index Copernicus
- Google Scholar
- The Global Impact Factor (GIF)
- Polish Scholarly Bibliography (PBN)
- Cosmos IF
- Open Academic Journals Index (OAJI)
- Directory of Research Journal Indexing (DRJI)
- EBSCO A-Z
- OCLC- WorldCat
- MIAR
- International committee of medical journals editors (ICMJE)
- Scientific Indexing Services (SIS)
- Scientific Journal Impact Factor (SJIF)
- Euro Pub
- Eurasian Scientific Journal Index
- Root indexing
- International Institute of Organized Research
- InfoBase Index
- International Innovative Journal Impact Factor
- J-Gate